Pharmacodynamics:
Lenalidomide is the leading compound of the new class of immunomodulators (IMiDsSM), which possesses both immunomodulating and anti-angiogenic properties.
Buy lenalidomide Price medications
-
 lenangio 25mg LenalidomideIn Stock: много
lenangio 25mg LenalidomideIn Stock: много -
 lenangio 10mg LenalidomideIn Stock: много
lenangio 10mg LenalidomideIn Stock: много -
 lenangio 5mg LenalidomideIn Stock: много
lenangio 5mg LenalidomideIn Stock: много -
 Lenalid 25mg LenalidomideIn Stock: много
Lenalid 25mg LenalidomideIn Stock: много -
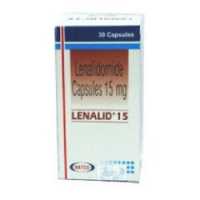 Lenalid 15mg LenalidomideIn Stock: много
Lenalid 15mg LenalidomideIn Stock: много -
 Lenalid 10mg LenalidomideIn Stock: много
Lenalid 10mg LenalidomideIn Stock: много -
 Lenalid 5mg LenalidomideIn Stock: много
Lenalid 5mg LenalidomideIn Stock: много
Lenalidomide
Pharmacodynamics:
Lenalidomide is the leading compound of the new class of immunomodulators (IMiDsSM), which possesses both immunomodulating and anti-angiogenic properties.
Lenalidomide inhibits the secretion of proinflammatory cytokines, including tumor necrosis factor, interleukin-1β, IL-6 and IL-12, from liposaccharide-stimulated peripheral blood mononuclear cells. Lenalidomide increases the production of the anti-inflammatory cytokine IL-10 and liposaccharide-stimulated peripheral blood mononuclear cells, as a result of which the expression, but not the enzymatic activity of cyclooxygenase-2, is inhibited. Lenalidomide induces the proliferation of T-cells and increases the synthesis of IL-2 and interferon-1ɤ, and also increases the cytotoxic activity of its own killer cells. Lenalidomide inhibits the proliferation of cells of various hematopoietic tumor lines, mainly those that have cytogenetic defects of chromosome 5. Lenalidomide inhibits angiogenesis, blocking the formation of microvessels and endothelial channels, as well as the migration of endothelial cells on the model of angiogenesis in vitro. In addition, lenalidomide inhibits the synthesis of proangiogenic vascular endothelial growth factor by means of PC-3 prostate tumor cells.
Pharmacokinetics:
Lenalidomide is a racemic mixture of two optically active forms: S (-) and R (+) with a total optical rotation equal to zero.
After oral administration, lenalidomide is rapidly absorbed; The maximum concentration is reached after 0.6-1.5 hours after a single dose. Meal does not affect the degree of absorption. The pharmacokinetic distribution is linear. The maximum concentration (Cmax) and the area under the concentration-time curve (AUC) increase in proportion to the dose increase. Repeated doses of the drug do not lead to its cumulation. In patients with multiple myeloma, lenalidomide is rapidly absorbed, with the maximum concentration being reached within 0.5-4.0 hours after administration, both on the first day and on the 28th day. Сmax and AUC increase proportionally with both single and repeated administration of the drug. According to Сmax and AUC, the exposure of lenalidomide in patients with multiple myeloma is higher than in healthy volunteers, which is explained by a lower clearance to filtration ratio in patients with multiple myeloma compared with healthy volunteers (300 and 200 ml / min, respectively). In vitro binding of (14C) -lelenomidom with plasma proteins of patients with multiple myeloma and healthy volunteers was 22.7% and 29.2%, respectively. Approximately 60% of lenalidomide is excreted by the kidneys unchanged. This exceeds the speed of glomerular filtration and, therefore, the process is both passive and active. The half-life of the drug increases with increasing dose, from about 3 hours at a dose of 5 mg to about 9 hours at doses of 400 mg. The equilibrium state is reached on the 4th day. The pharmacokinetics of lenalidomide have not been studied in patients with impaired liver function. In patients with impaired renal function, the absorption of lenalidomide does not change.
Indications:
Treatment (in combination with dexamethasone) in patients with multiple myeloma who have received at least one line of therapy.
ICD-10
Contraindications:
Pregnancy; lactation period (breastfeeding); childbearing age; the inability to comply with the necessary contraceptive measures; childhood; hypersensitivity to lenalidomide.
Carefully:
Elderly patients with renal insufficiency; patients with multiple myeloma who take lenalidomide together with dexamethasone, as drugs with erythropoietic activity, as well as hormone replacement therapy may increase the risk of thrombosis.
Pregnancy and lactation:
Contraindicated use during pregnancy and lactation (breastfeeding).
Lenalidomide is a structural analogue of thalidomide, which has a pronounced teratogenic effect. It is known that taking thalidomide in pregnant women causes severe and life-threatening disorders of the internal organs of the fetus (with a frequency of up to 30%). Experimental studies on monkeys showed results similar to the previously described results for thalidomide. The risk of birth defects is very high if lenalidomide is used during pregnancy.
Strict adherence to contraception applies to women and men.
FDA Category X recommendations.
Dosage and administration:
Take inside.
The recommended initial dose is 25 mg 1 time per day on the 1-21st day of repeated 28-day cycles. Dexamethasone at a dose of 40 mg is prescribed 1 time per day in the 1-4th, 9-12th and 17-20th days of each 28-day cycle during the first 4 cycles of therapy, and then 40 mg each 1 once a day on days 1-4 of each subsequent 28-day cycle.
With the development of toxic effects, the dosing regimen is adjusted according to a special scheme.
In patients with impaired renal function, correction of the dosing regimen is required.
Side effects:
The most severe adverse reactions are: venous thromboembolism (deep vein thrombosis, pulmonary thromboembolism), grade 4 neutropenia.
On the part of the hematopoietic system: very often - neutropenia, thrombocytopenia, anemia; often - leukopenia, lymphopenia.
Since the cardiovascular system: often - deep vein thrombosis, lowering blood pressure.
Infections and invasions: often - pneumonia.
From the musculoskeletal system: very often - muscle cramps.
On the part of the nervous system: often - tremor, hypoesthesia.
On the part of the respiratory system: often - shortness of breath (including during exercise).
From the skin and subcutaneous fat: very often - skin rash; often itchy skin.
General reactions: very often - weakness, asthenia.
Most often when using the combination lenalidomide + dexamethasone: neutropenia (39.4%), muscle weakness (27.2%), asthenia (17.6%), constipation (23.5%), muscle cramps (20.1%) , thrombocytopenia (18.4%), anemia (17%), diarrhea (14.2%), rash (10.2%).
Overdose:
A special plan of action for overdose of lenalidomide in patients with multiple myeloma is not currently developed, despite the fact that some patients received doses up to 150 mg in dose range studies, and up to 400 mg in single dose studies. Toxic manifestations that limited the dose in these studies were exclusively hematological.
Treatment: in case of overdose, symptomatic supportive therapy is recommended.
Interaction:
Erythropoietic drugs, as well as other drugs that may increase the risk of thrombosis, such as drugs for hormone replacement therapy, should be used with caution in patients with multiple myeloma who take lenalidomide in combination with dexamethasone.
Mutual influence on the metabolism of lenalidomide and other drugs is unlikely due to the fact that lenalidomide is not metabolized by the cytochrome P450 system.
Digoxin
The simultaneous appointment of lenalidomide with digoxin is accompanied by an increase in the plasma concentration of digoxin. During treatment with lenalidomide, it is recommended to monitor the concentration of digoxin.
Oral contraceptives
Dexamethasone, which is an essential component of a lealidomide treatment regimen, may decrease the effectiveness of oral contraceptives. To effectively prevent pregnancy, it is necessary to use the means specified in the Pregnancy Prevention Program.
Warfarin
Mutual effect on the pharmacokinetic parameters of lenalidomide and warfarin was not observed. Given the use of dexamethasone in combination with lenalidomide, the effect of the latter on the effects of warfarin cannot be excluded. Thus, against the background of combination therapy with lenalidomide and dexamethasone, careful control of the concentration of warfarin is recommended.
Special instructions:
For the prevention of venous thromboembolism, especially in patients with additional risk factors, the use of low molecular weight heparins or warfarin is recommended. The decision on the appointment of antithrombotic therapy should be made after a thorough assessment of individual risk factors.
The risk of developing neutropenia 4 severity in patients with multiple myeloma with simultaneous use of lenalidomide and dexamethasone is very high.
It is recommended that both the doctor and the patient closely monitor the symptoms of increased bleeding, including petechiae and hemoptysis.
During the first 2 months of treatment with lenalidomide, it is recommended to perform a detailed blood test every week, including determining the number of leukocytes, blood formulas, platelet count, hemoglobin, hematocrit. In the subsequent blood tests should be performed monthly.
The manifestations of lenalidomide toxicity, which most often limit its use, include neutropenia and thrombocytopenia. In this regard, the decision on the joint use of lenalidomide and other immunosuppressive drugs should be clinically justified.
Considering the preferential excretion of lenalidomide by the kidneys, in patients with renal insufficiency, it is necessary to carefully monitor the state of renal function and the dose of lenalidomide.
Regular monitoring of thyroid function is necessary due to the possibility of hypothyroidism under the influence of lenalidomide.
It is impossible to exclude the possibility of the neurotoxic action of lenalidomide during its long-term administration, taking into account the structural similarity of the molecules lenalidomide and thalidomide, which is known for its pronounced neurotoxic side effect.
Due to the pronounced antineoplastic activity of lenalidomide, tumor lysis syndrome may develop, especially in patients with a large tumor mass. The condition of such patients should be monitored and appropriate prophylaxis carried out.
Patients are not allowed to donate blood or semen as a donor during the entire treatment with lenalidomide and for one week after its termination.
Influence on ability to drive motor transport and control mechanisms
Some side effects of lenalidomide, such as dizziness, weakness, drowsiness, and blurred vision, can adversely affect the ability to drive and perform potentially hazardous activities that require increased concentration and psychomotor reactions. In this regard, when driving and working with mechanisms should be especially careful.
